Brain Organoids
ENDLESS POTENTIAL
Brain Organoids empowering Drug R&D
Although brain diseases are a global crisis, there are no cures
To stem the rising tide of disability caused
by brain disease in increasingly aging
populations, innovative approaches for
Drug R&D are urgently needed.
Currently it takes 10 ‒ 15 years for a new drug to reach patients. Due to an attrition rate of > 95%, drug development is expensive (> $ 2 billion per drug reaching the market).
Some already approved drugs have to be withdrawn from the market, and drug developers face high multi-million to multi-billion dollar indemnity payments for damages caused by side effects.
Due to a lack of adequate models for the human nervous system, toxicity to the nervous system (neurotoxicity) was the
4th reason of withdrawals.
The complexity of the human brain leads to a particularly high failure rate for brain disease therapeutics, as here toxicity is the least predicted by animal experiments. Only 1/5 drug candidates toxic to the brain are picked-up in animal experiments. The other 4/5 proceed into human trials and are toxic to the trial participants.
Effectiveness of brain disease drug candidates is also problematic:
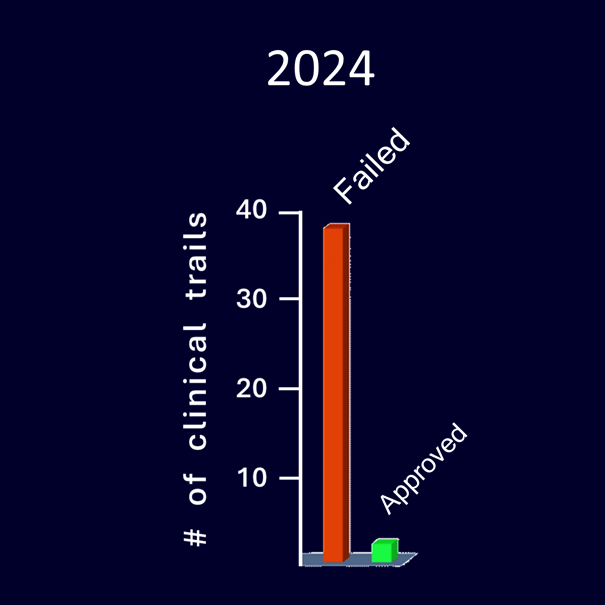
In 2024 alone, 37 clinical trials for brain disease drugs were stopped and only 2 new drugs were approved.
Cell Biology 101
&
ORGANOIDS
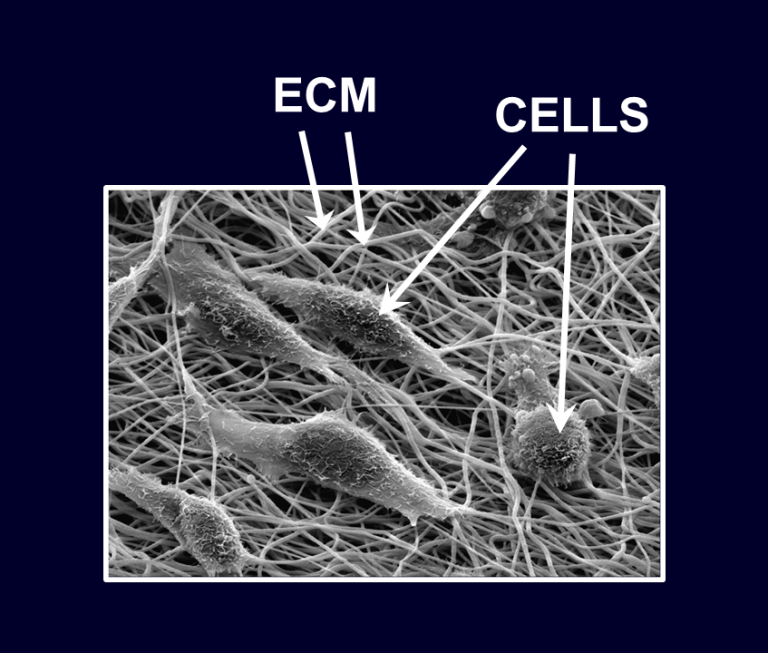
Organs in the body always consist of different cell types, all important for proper functioning of the organ. The three-dimensional organ structure is uphold by a scaffold, the so-called extra cellular matrix (ECM), a mixture of proteins and other molecules. All cells are in direct contact with the ECM and other cells. Long thought to provide only structure, it has emerged in recent years that the ECM also relays signals from the environment, deep into the cell. Similar to a spider’s web transmitting the wiggling of an entrapped insect, the ECM transmits signals to the embedded cells.
In addition to this, cells communicate with each other via messenger molecules such as cytokines, interferons, growth factors and other molecules. They even release little capsules called extracellular vesicles (or exosomes), packed with RNA, DNA, fat molecules, and proteins. The extend and exact function of these vesicles is still not fully understood.
With the exception of a few stem cells that maintain the organ by generating new cells to replace old cells that died, these new cells do not divide once they are fully matured.
All these highly tuned processes maintain homeostasis of the organ and prevent cells to turn ‘rogue’ and start tumors. Accordingly, cells taken out of an organ do not grow easily in a culture dish. On the other hand, cells rogue from tumors can endlessly grow in culture.
Human Cells in the Dish
As human material is scarcely available, since decades research has used human cell generated from tumors and normal cells isolated from animals. However, human tumor cells, which are full of mutations, or mouse cells and are not necessarily reflecting normal human cells.
With improvements in cell culture it has become possible to coax normal human cells to divide to some extent in the dish. However, for drug R&D, requiring cells to test millions of molecules, this is by far not enough. Thus, human therapies are mostly developed on human degenerated cells, animal cells (usually from mice) and animal models.
Over the years it has emerged that such models are not physiologically relevant for the human organism. The outcome in drug R&D is that there are no cures, many drugs are poorly effective, and side effects can be strong, sometimes even deadly.
The Role of Stem Cells
Like normal human cells, tissue stem cells do not grow to large amount in culture.
The availability of so-called pluripotent stem cells (PSC) such as human embryonic stem cells and iPSC, for the first time in history enables the generation of large quantities of normal human cells in the dish. Moreover, PSC can generate all types of cells in the body, in large quantities. As such, for the first time, normal liver cells, brain cells or even heart cells from human can be generated in the dish to support drug R&D.
Organoids, a new Horizon in Human Healthcare
Important progress has been made since the availability of stem-derived normal human cells and much new knowledge has been gained. Including that humans are different from mice and other laboratory animals. If we were mice, we would not reject transplanted organs, have no autoimmune disease, no diabetes, no obesity, no heart or liver disease.
Decades ago, it was discovered that cells thrive in three-dimensional (3D) cell culture environments.
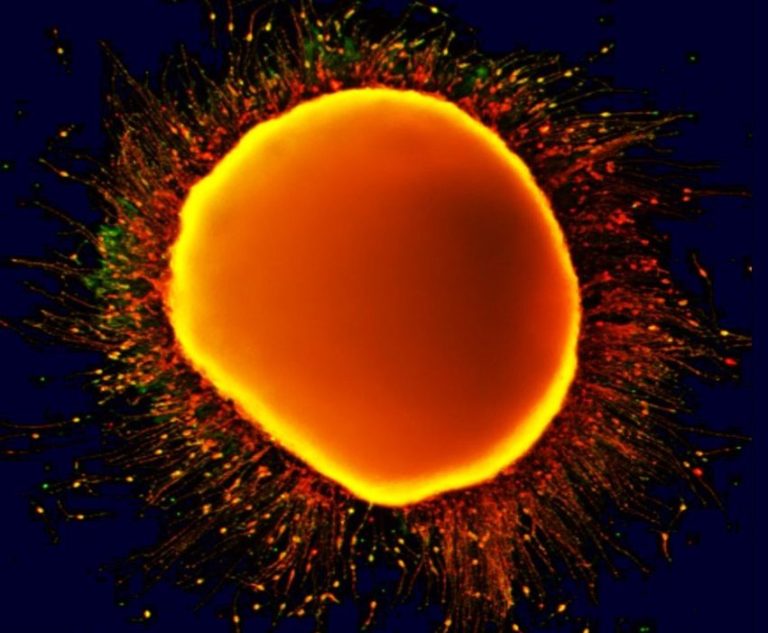
The availability of PSCs and their inborn inclination to form all types of cells in the dish now enables the creation of 3D cellular structures resembling organs. In fact, under the right conditions, PSCs form these structures entirely on their own, creating ‘mini-organs’ containing multiple different cell types — organoids.
It is becoming increasingly clear that they are ideal to investigate human-specific cellular functions, organ function and with that disease aspects.
Lack of adequate models is particularly relevant for the human brain, which is the most complex among mammals, and is particularly poorly modelled with mice or rats. Accordingly, medications for brain diseases are not working well in humans and their development is risky for pharmaceutical companies. For drugs for brain disease, problems are often only detected when the candidate drugs transit from animal safety testing into humans. Only 20% of the safety failures occur in animal safety testing prior to clinical trials. The other 80% are occurring in humans. Moreover, a large majority of the drugs that continue in clinical trials, later fail due to lack of effectiveness.
The Journey Has Started
Brain Organoids
It is now possible to develop therapies for the almost 30% of the global population suffering from brain diseases.
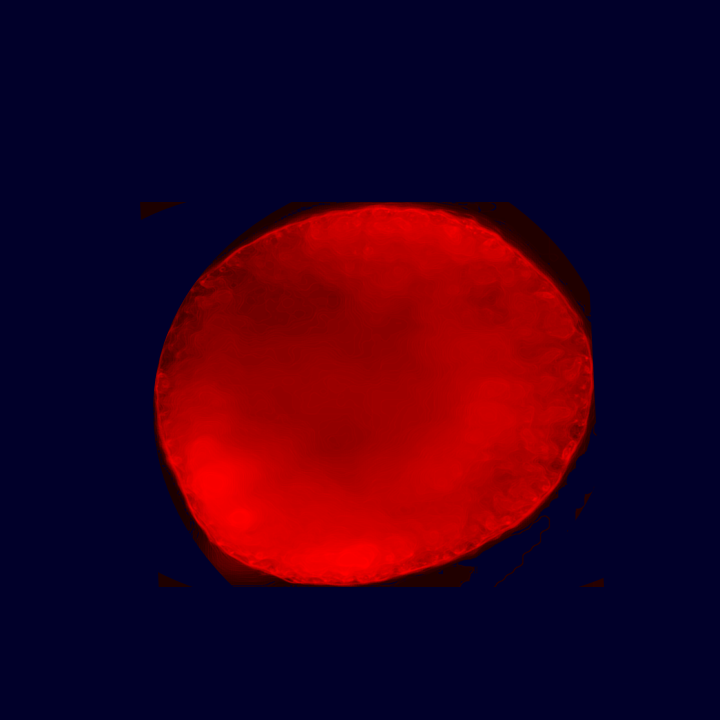
With our brain organoids we have already shown in 2012 that nano-plastic (made of polyethylene like in plastic bags) accumulated in brain tissue.**
This was recently corroborated by real life data, in a publication in Nature Medicine. The authors found an accumulation of nano-sized plastic, in large part polyethylene, in the brain of deceased humans. This accumulation was particularly high in brains of dementia patients.***
** Hoelting et al., Archives of Toxicology, 2012 ***Nihart et al., Nature Medicine, 2025
Brain organoid filled with red nano- particles made of polyethylene
plastic, after 48 hours of exposure.
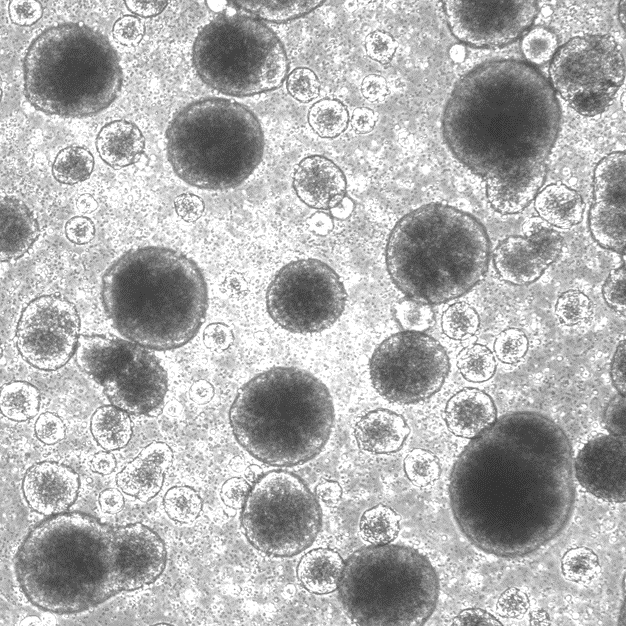
Brain organoids are expected to reduce these problems significantly, as they are the closest model for the human brain available. It is now possible to identify the exact mechanisms underlying major brain diseases* such as Alzheimer's disease and other dementias, Parkinson's disease, depression, multiple sclerosis, ALS, autism and other mental illnesses.
*https://my.clevelandclinic.org/health/diseases/22934-brain-diseases
OUR MISSION
nostro discovery's mission is to accelerate & de-risk drug developement with its innovative brain organoids and to
empower the development of cures for the almost 30% of the global population suffering from brain diseases.
Have any questions? We are always open to talk about your business, new projects, creative opportunities and how we can help you to de-risk your pipeline and reach market faster.
